The 2019 Novel Coronavirus, also known as SARS-CoV-2, caused an outbreak of respiratory illness called COVID-19, in Wuhan, China. It has since spread to other parts of China and the world. Coronaviruses are a family of viruses that infect birds and mammals (this includes humans!). Typically, they cause mild respiratory symptoms similar to the common cold, but can lead to death, often in those that are already immunocompromised.
Quick look : How does COVID-19 compare to the other coronaviruses?
SARS
2002
In 8 mo
8,000
confirmed cases
9.6%
death rate
MERS
2012
In 36 mo
2,484
confirmed cases
34.4%
death rate
COVID-19
2019–Present
So far in 73 mo
0.00
confirmed cases
NaN%
death rate
Live update of COVID-19 numbers
How deadly is COVID-19?19,20
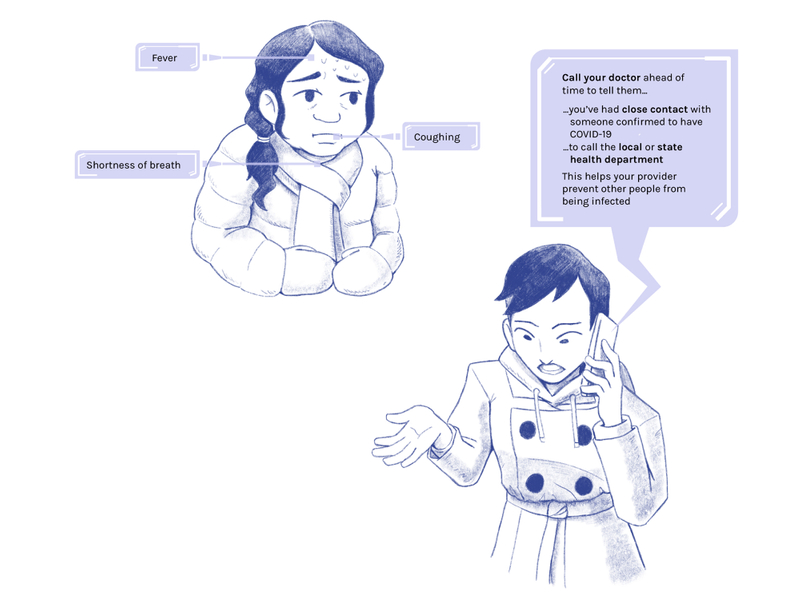
While COVID-19 is much more infectious, it appears to be less deadly than SARS or MERS right now. However, it is more deadly than the annual flu, which has a death rate of less than 1%. This is why it is even more important that if you experience mild symptoms, you should seek medical care right away, and practice hygienic habits to slow the spread of germs and COVID-19 to the people around you.
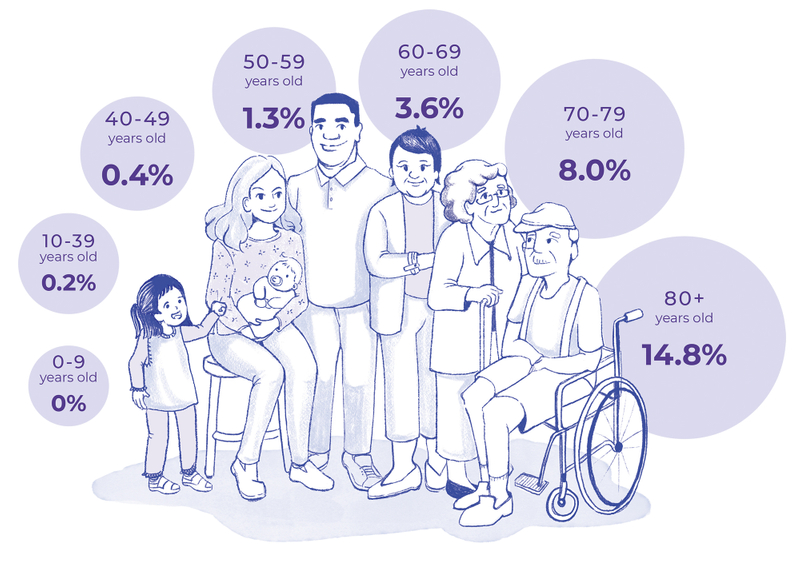
China's COVID-19 death rate by age as of 11 Feb 202019,20
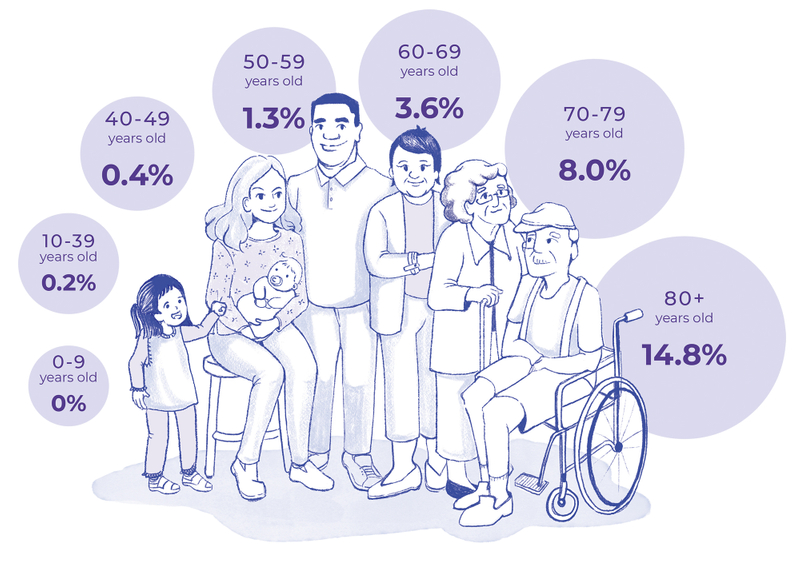
Note: Diseases do not have a single case fatality rate; it depends on context, and changes with time and location.
1 Dec 2019
First patient confirmed in Wuhan, China
31 Dec 2019
China sends urgent notice to WHO of unknown respiratory illness cause
7 Jan 2020
- New virus identified as a coronavirus
- Europe's first case confirmed in France
11 Jan 2020
First death is announced in China
21 Jan 2020
First case in the US is confirmed; Snohomish County, Washington
24 Jan 2020
First case of human-to-human transmission is confirmed outside of China in Vietnam
30 Jan 2020
- WHO declares the outbreak a global public-health emergency (PHE)
- The US reports the first confirmed instance of person-to-person spread
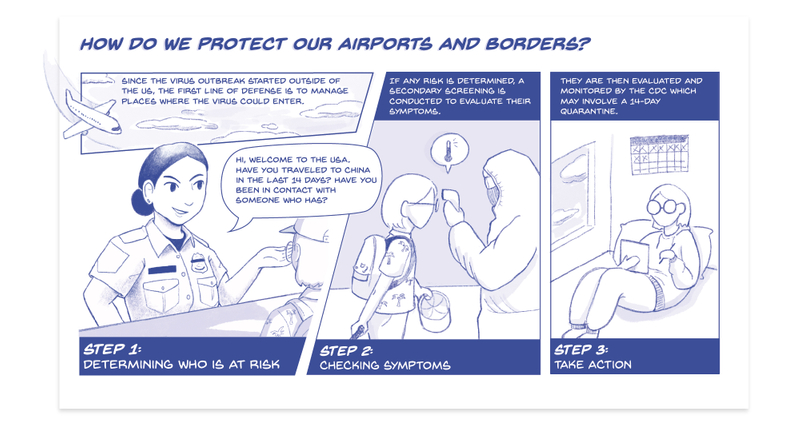
31 Jan 2020
- HHS Secretary declares a PHE for the US
- President Trump enforces a 14-day quarantine preceding the entry of travelers from mainland China into the US
11 Feb 2020
WHO announces a new official name for the disease as "COVID-19"
25 Feb 2020
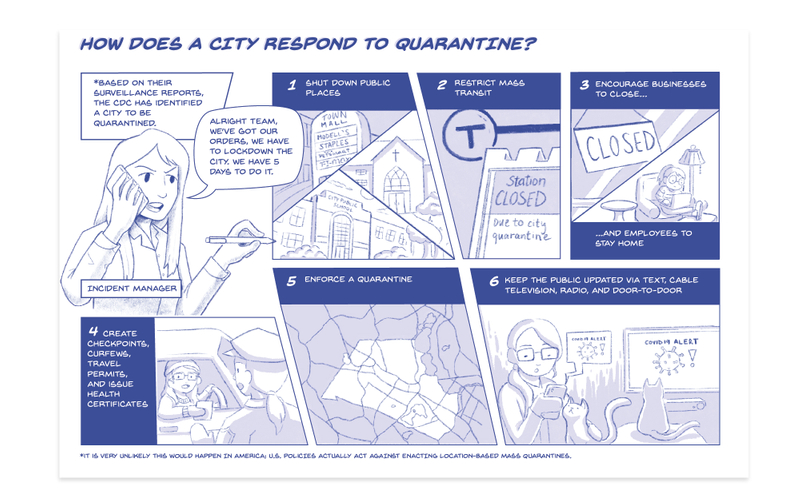
CDC warns community to prepare for the spread of COVID-19 in the US
29 Feb 2020
First death in the US in King County, Washington
1 Mar 2020
UN releases $15 million USD from the Central Emergency Response Fund (CERF) to fund global efforts to contain the virus
11 Mar 2020
WHO announces that the COVID-19 outbreak is a global pandemic
13 Mar 2020
President Trummp declares a National Emergency, allowing those in charge to act faster in response to an emergency
What happens now?
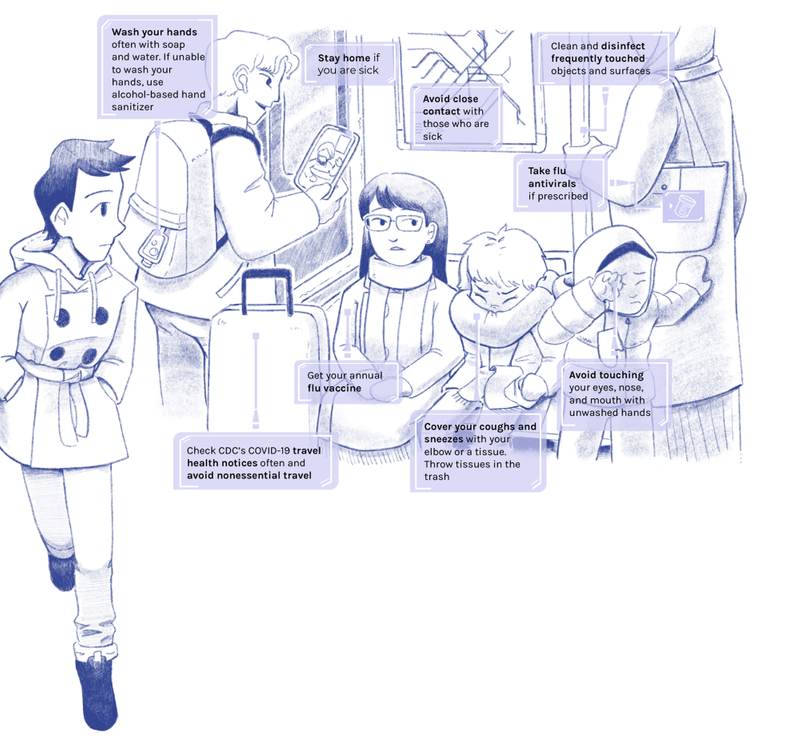
COVID-19 has spread from Asia to North America, South America, Europe, Oceania, and Africa. The world continues to work towards treating the sick and containing the disease as we learn more about it. For now, the public is encouraged to practice social distancing and hygienic practices.
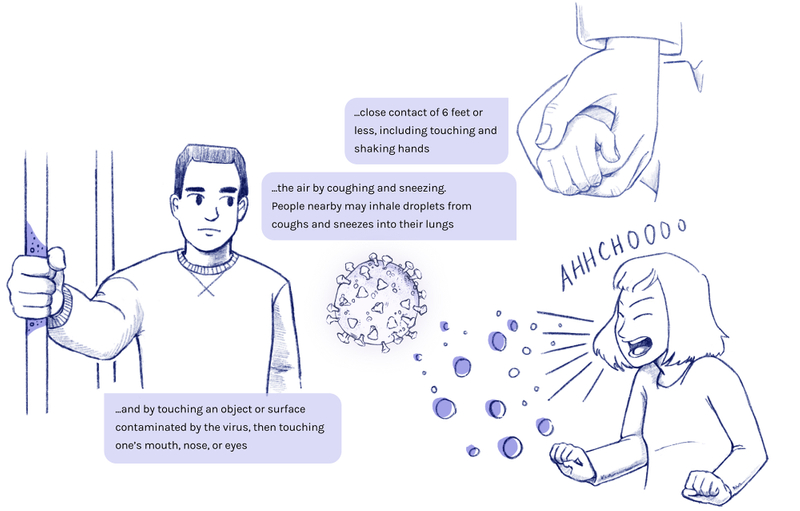
At this time, we don't know how fast or easily this virus is spreading between people. More information is discovered everyday, but here's what we know so far.
Human-to-human transmission is possible
The virus first came from an animal source, but it is now able to spread from human to human.
It travels through droplets in the air
It can infect humans through...

...close contact of 6 feet or less, including touching and shaking hands.

...the air by coughing and sneezing. People nearby may inhale droplets from coughs and sneezes into their lungs.

...and by touching an object or surface contaminated by the virus, then touching one's mouth, nose, or eyes.
Incubation Period9
The time between exposure to the virus and the start of symptoms is between 5.2 - 12.5 days.