Physician Burnout: The Silent Killer
Physician burnout is a public health crisis.1 We're losing physicians to burnout, drop out, and suicide. The suicide rate alone in 2018 was at a rate of 28 to 40 per 100,000, triple the national average19 . By 2032 with the status quo we will have 2.37 physicians to every 1000 patients, and with early retirement that number will drop even further to 2.25 physicians per 1000 patients.9 This is a respective 4% and 8% decline in the physician-to-population ratio (declining from 2.47 physicians per 1000 patients in 2017).
Physician burnout is a problem that has been recognized for decades. More than half of physicians experience symptoms of burnout, a rate nearly double of workers in other professions after taking into account hours, work, age, sex, and other factors.3 Burnout is identified in physicians as emotional exhaustion, depersonalization, cynicism, and job dissatisfaction,1 and can lead to physical exhaustion, feelings of failure, social isolation, conflicts with colleagues, poor clinical performance, depression, and substance abuse or self-medication.14
Covid-19 is intensifying the burnout crisis
Pre-covid, we began 2020 with unprecedented rates of clinical depression and suicide in the physician and, in fact, the entire US healtcare workforce. With the Covid-19 global pandemic making waves through the world's healthcare systems, more healthcare workers than ever are on the front-lines, putting themselves at risk to save lives and beat this virus. They are working long hours, with limited resources, and the added burden of sourcing PPE for their own safety. Healthcare workers expressing concerns and advocating for safety are silenced and often retaliated against, by way of termination of employment, when they do speak up. Eric Topol, MD sums it up best in a perspective piece, US Betrays Healthcare Workers in Coronavirus Disaster, published in Medscape.
What the research shows
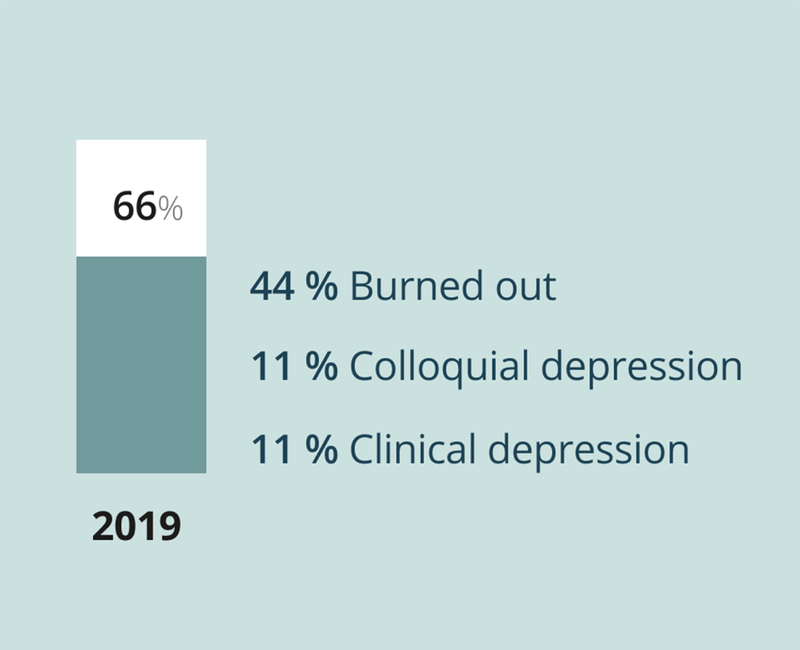
Depression & Suicide Report
Per a 2019 Medscape National Physician Burnout, Depression & Suicide Report, 66% of physicians reported feeling burned out (44%), colloquial depression (11%), or clinical depression (11%).16
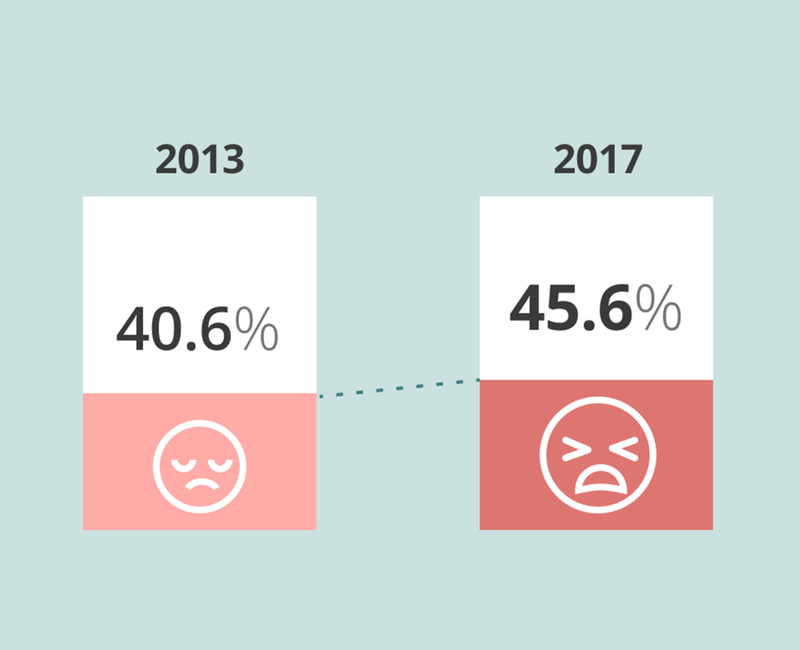
Burnout in Academic Physicians
In an academic medical faculty practice study administered to 1,774 physicians in 2014 and 1,882 physicians in 2017 burnout increased from 40.6% (720) to 45.6% (858).5
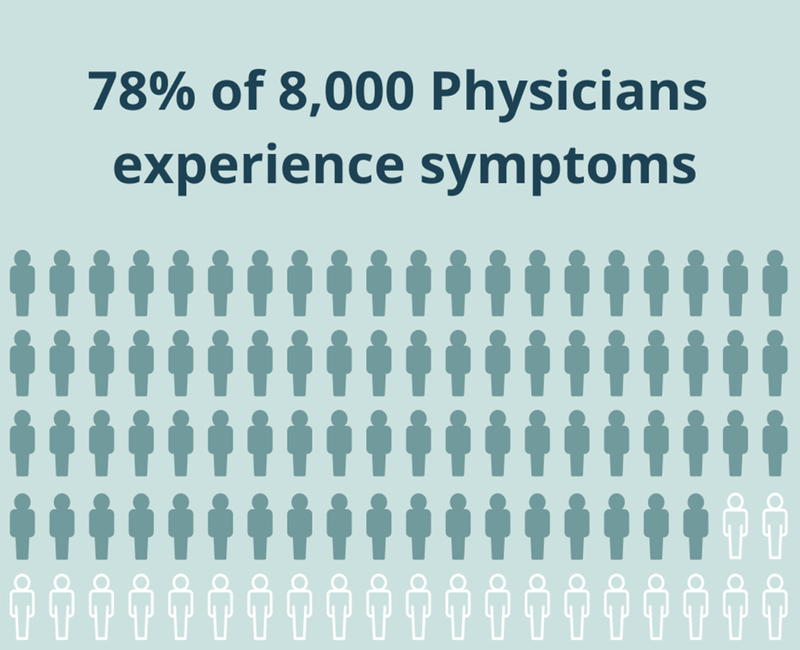
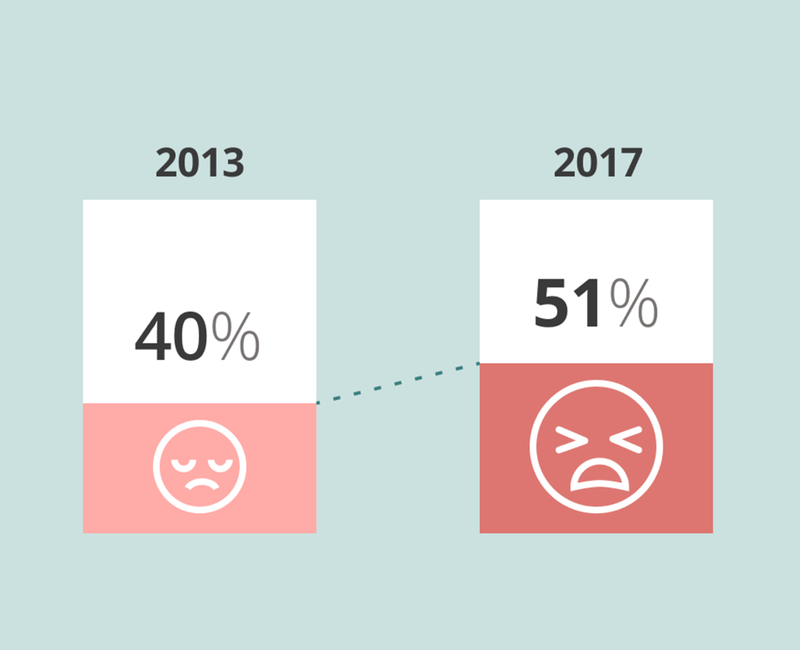
Physicians with Symptoms
A 2018 Survey of America's Practice Patterns and Perspective conducted by Merritt Hawkins found that 78% of over 8,000 physicians experience symptoms of burnout at least once in their career.6 Typically, once experienced, symptoms of burnout will return over the course of a career.
Research does not say it all
Although a recent study published in Mayo Clinic Proceedings7 reported a decline in physician burnout at a rate below 50%, its optimistic conclusions are premature. It concluded "burnout and satisfaction with Work Life Index (WLI) among US physicians has improved between 2014 and 2017. This trend is reason for optimism and suggests that progress is both possible and under way." As of 2016 there were over 950,000 actively licensed physicians in US.8 In the study, only 5,207 physicians responded, representing a mere 0.54% of these physicians. Physicians working the front lines of care, especially female physicians, are at a greater risk for burnout; yet these physicians were underrepresented. The majority of respondents were male, and only 23.8% physicians surveyed were in primary care. Evidence shows that female physicians, as well as those in primary and urgent care, are more at-risk for showing signs of burnout. Additionally, the study only captured a single snapshot rather than a longitudinal measurement of burnout. Despite the report of improvement in WLI satisfaction regarding burnout, the number of physicians who screened positive for depression increased from 38.2% in 2011 to 39.8% in 2014 and to 41.7% in 2017. Work-related risk factors for burnout are predictors of depression. The improvement seen in burnout and WLI is likely a result of the desire to provide acceptable answers, under-report symptoms of burnout, and downplay the significant attrition of the physician workforce from 2011 to 2017.
Physician burnout is worsening, and will continue to do so for the foreseeable future. A report by AAMC (Association of American Medical Colleges) has projected that physician demand will increase faster than supply and has projected a shortage of 122,000 physicians by 2032.9 Signs of burnout have been identified at all levels of medical training, with emotional distress in residency leading to emotional exhaustion and depersonalization later in career.14 Burnout isn't limited to starting out as a physician. Once symptoms are experienced, they will surface again and again and stay with a physician throughout their career. Physicians experiencing burnout symptoms are likely to reduce their hours, change specialties, or leave healthcare altogether, costing approximately $160,000 to $1,000,000 to replace a single physician, leading to $4.6 billion yearly in the United States.10,14 Its impact extends beyond physicians and their employers and affects us all. Fewer physicians in practice can mean longer wait times for patients, shorter visits, and dissatisfaction with care.
Further evidence links burnout with increasing medical errors.11 Additionally, physicians experiencing burnout are twice as likely to be affected by patient safety incidents, twice as likely to deliver suboptimal care to patients due to low professionalism, and three times more likely to receive low satisfaction ratings from patients.18 Patients on the receiving end of erroneous care will no longer trust their attending physician, leading to reduced compliance of following prescribed therapies, distrust of the medical and healthcare system as a whole, and added pressure on the clinician.
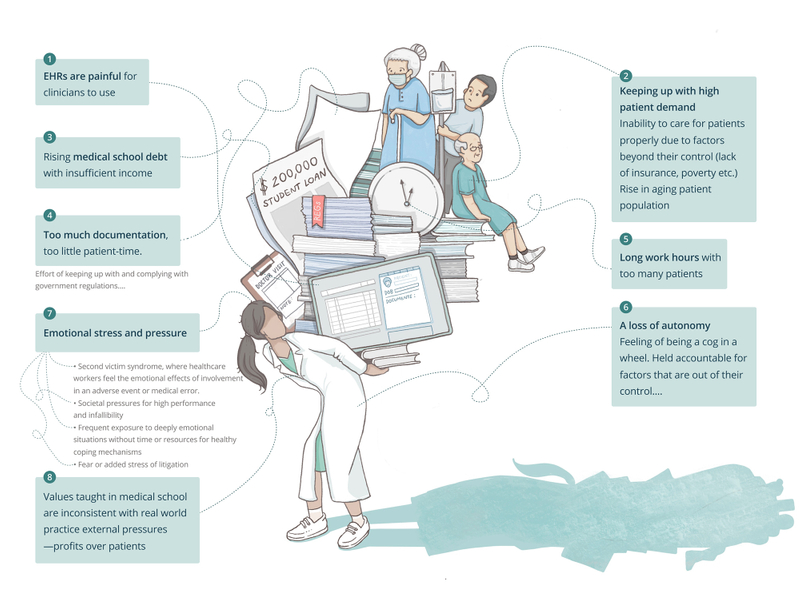
Contributors to Burnout14,15
There are many contributing factors that put healthcare workers at risk of burnout, including but not limited to those listed below. To get at root causes of burnout and the symptoms leading up to them, comprehensive qualitative studies are needed with proper representation across all of healthcare. This is no easy task, but until it is done, we will have an incomplete picture of physician burnout.
What we can do about it now
Rather than paying lip-service to a chronic and escalating crisis, we need to see action toward measurable change and sustainable solutions. By looking at the contributors, we have specific targets for change, as well as systemic change that would greatly reduce the burden put upon physicians and health care workers. We can do this in small ways, by giving patients and physicians more tools for remote care, with the use of telemedicine, at-home or time-of patient-reported outcomes (PROs) to track the health of a patient in real time, and the recording and analysis of those outcomes to become predictors of our health.
Organization-oriented approaches for better interventions
The term "burnout" itself and its medicalization is problematic and minimizes the role of systemic factors. Burnout is an outcome rather than root cause of issues in our healthcare system, as a result of complex interactions between environmental, genetic, demographic, and psychosocial factors. The understanding of how these factors influence burnout is critical to customizing interventions rather than the current one-size-fits-none model.
Eliminate the stigma
There is a value mismatch between organizations and physicians, in which the business of healthcare does not align with the practice of medicine. Medicine was once a profession and beyond medical school it has evolved to become the business of healthcare. In the business of healthcare, physicians are known as providers, ability to pay matters, and efficiency trumps empathy. The start of medical school begins with the hippocratic oath where physicians are taught to do no harm and care for all patients equally and without discrimination. Physicians are ensnared in a perpetual dilemma between ethics of medical training, patient health, and the realities of a business that profits when people are extremely ill and incredibly vulnerable. Because the number of physicians with symptoms of burnout is so high, it is unlikely that the origin of the issue is in the susceptibility of individuals, rather it is rooted in the environment and care delivery system.14 It is precisely why individual measures alone have failed to address the problem. Organization-oriented approaches are more effective than individual ones according to a systematic review analyzing individual and organizational strategies.13
In terms of psychosocial factors, stigma and punitive measures associated with mental illness must be eliminated. Physicians who suffer from mood disorders are often reluctant to admit it or seek treatment because they are subject to unjust dire consequences such as career jeopardy, revocation of license to practice by state medical boards, and retaliation, rather than support, from employers, state boards, professional organizations, and peers. Historically, it has been the norm to hold those in the medical profession to infallible and superhuman standards. Presently nothing has changed; burnout is viewed as a sign of personal weakness or failure in the profession,14 leading to many symptoms and cases going underreported. Fear of litigation is a disabling affliction. This culture shift is critical if we are ever to reduce burnout. Physicians would rather quit medicine than report burnout or symptoms of burnout.
Defining the problem, both at an individual and systemic level, and utilizing accurate measurement tools would be a starting point. Burnout is now a legitimate medical diagnosis per the International Classification of Diseases (ICD-11) and the World Health Organization's (WHO) clinician handbook but there is no consensus on the measurement of burnout.12 The most commonly used measure of burnout is the Maslach Burnout Inventory (MBI) which was designed as a research tool, rather than a diagnostic and clinical tool. Create a reportable quality of life measure for physicians that can't be used to determine clinical quality. With destigmatization, more accurate reporting can lead to real change in healthcare culture that will reduce healthcare worker burden.
Physician-friendly EHRs
It is imperative that all healthcare stakeholders be held accountable for their contributions, especially health technology companies, their investors, as well as policy makers and regulators. While the roots of burnout predate the routine use of electronic health records (EHRs), there is wide consensus that frustration with EHRs is the top contributor to physician burnout. While relying on EHRs has made strides in healthcare delivery efficiency, software is still prone to glitches and performance issues. A note that may have taken upwards of 15 minutes to compose can be wiped out in microseconds due to poor UI design or malfunction. Frustrations with EHRs aren't limited to software issues. From the beginning, EHRs were designed to optimize billing and maximize reimbursement —not for patient care. Yet healthcare technology continues to "innovate" at lightning speed and with minimal consideration of their end users, physicians and patients.
There are many technology solutions claiming to be the magic pill to cure burnout. However, the majority of these solutions are created without a thorough understanding of the physician needs and pain points. It adds fuel to the fire, further intensifying the burnout crisis. Co-design with physicians, nurses, and patients, to intentionally create experiences patient safety and experience in mind for people, rather than designing healthcare around them.
The self-documenting encounter
Use audio and visual recording to passively document encounters and reduce how much time physicians spend at the keyboard with administrative tasks, buried in software. The physician would use voice commands and structured keywords to trigger orders and actions, query and input key information into the medical record as structured data or documentation of the clinical encounter. The self-documenting encounter will be finely tuned and evolve to become the defacto way to seamlessly capture information each visit. Physicians will spend less with fingers to keyboard and nose to screen and more face time with the patient.
National licensing will expand physician reach
Physicians who work for hospitals and independent practitioners who want to bill insurance must undergo licensing, credentialing, certification, and privileging. As an independent practitioner who does not bill insurance, at the very least one must be licensed and certified. Medical licenses are only valid in the state in which one is licensed except if one works for the federal government organization, such as the Veterans Affairs (VA) System, then a valid license in one state is valid nationwide. There is no standardized process or central licensing system. The state by state requirements and processing times highly vary. At present clinicians need to jump through hoops to be certified, licensed, credentialed, and privileged, making the option to leave clinical medicine more appealing. There is decentralization and fragmentation of the process. One nationwide license and eliminating state-by-state licensing will allow physicians to practice between state lines including telemedicine which has proven to be a critical resource during the current viral pandemic. Additionally, a single national provider network with a searchable national provider database needs to be created in place of the current repository of National Provider Identification, NPIs which are unsearchable and incomplete.
Evolve medical education
Medical education curriculum needs reform and to move away from strictly a biological health-disease model to one that is comprehensive to also include psychological, social, cultural, and economic components of medicine. 11% of health is medical care and 89% occurs outside the clinical space. Courses in the business of healthcare need to be mandatory so new graduates are skilled to navigate the complexities of the business of healthcare.
Skyrocketing costs of education also need to be addressed. Per AAMC 2019 report, the cost of medical education tuition and fees ranges from $37,556 (public, in-state) to $62,194 (public, out-of-state) yearly and with private school figures ranging from $60,665 and $62,111 per year.17 Surgical specialties compensate far greater than their non-surgical counterparts and specialists are better rewarded than generalists and primary care physicians. Physicians lag a decade in earnings as compared to their non-physician colleagues. In combination, these can lead physicians to pursue post-graduate training in more financially lucrative specialties to pay off an insurmountable debt.
More work is needed
These ideas illustrated above are by no means the end to what needs to change in the United States healthcare system. Our hospital system is strained, we have too many patients per clinician, and the few clinicians we have are not getting the support they need. Despite that, the healthcare industry is growing everyday, with new players entering some with innovative ideas, all with conflicting interests, whether regulatory, data-centric, or profit-oriented, where the number of patients per day are the bottom line. In the end, patients are the subjects of care, and the outcomes of their care is what matters. Asking physicians to juggle all the interests competing for attention in the healthcare industry is irresponsible.

The time to act is now
We need to give support and PPE to our physicians on the front lines during this public health crisis that is now further exacerbated by the Covid-19 pandemic. While dealing with nearly 900,000 confirmed Covid-19 cases in the US that are growing everyday (at the time this article was written), and dwindling to non-existent resources, healthcare workers have contracted the Covid-19 virus, and physician deaths have occurred with many more imminent. Many of these deaths could be prevented. The current death reports are an underestimate, limited by the testing shortage and lack of uniform collecting and reporting of data by state and federal agencies, including the Centers for Disease Control and Prevention.
The tide for the physician burnout crisis is not turning. Physician burnout is only the tip of the healthcare industry's sickness. Physicians will become scarce in ten years should we fail to end this epidemic with well-designed approaches addressing both individual and organizational needs. Patients unable to buy their way to the top may have to wait years for a routine surgery or it may be internationally outsourced. It is unacceptable that so many physicians are painfully suffering in silence and dying. Even one physician suicide is one loss too many.
Authors
Subscribe to our newsletter
You'll receive our latest ideas, visualizations, and studio news delivered to your inbox twice a month.
References
- Ashish K. Jha, MD, MPH, et al., A Crisis in Health Care: A Call to Action on Physician Burnout, Partnership with the Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T.H. Chan School of Public Health, and Harvard Global Health Institute. Accessed Mar 2020 (archived link): https://web.archive.org/web/20200413051545/http://www.massmed.org/News-and-Publications/MMS-News-Releases/Physician-Burnout-Report-2018/
- Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8; 172(18):1377-85.
- Paul Griner, Seth Bilazarian, Peter Moskowitz. May 2013. Medscape Physician Lifestyle Report 2013. Accessed Mar 2020: https://www.medscape.com/sites/public/lifestyle/2013
- Peckham C. Medscape Lifestyle Report 2017: race and ethnicity, bias and burnout. May 2018. Medscape Lifestyle Report 2017. Accessed Mar 2020.: https://www.medscape.com/features/slideshow/lifestyle/2017/
- Marcela Carmen. Factors Associated With Physician Burnout At an Academic Faculty Practice. Accessed Mar 2020.: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2727998
- Hawkins M. 2018 Survey of America's Physicians: Practice Patterns & Perspectives. 2018. Accessed Mar 2020. (original source no longer available): https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/MerrittHawkins_2018_Physician_Survey.pdf
- Shanafelt, Tait D. et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clinic Proceedings, Volume 94, Issue 9, 1681 - 1694. Accessed Mar 2020: https://www.mayoclinicproceedings.org/article/S0025-6196(18)30938-8/fulltext
- Aaron Young, et al. A Census of Actively Licensed Physicians in the United States, 2016. 2017. Federation of State Medical Boards. Accessed Mar 2020: https://www.fsmb.org/siteassets/advocacy/publications/2016census.pdf
- IHS Markit Ltd. The 2019 Update: The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. April 2019. Association of American Medical Colleges. Accessed Mar 2020 (original link no longer available): https://www.aamc.org/system/files/c/2/31-2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf
- Shasha Han, et al. Estimating the Attributable Cost of Physician Burnout in the United States. June 2019. Annals of Internal Medicine. Accessed Mar 2020 (archived link): https://web.archive.org/web/20200308090207/https://annals.org/aim/article-abstract/2734784/estimating-attributable-cost-physician-burnout-united-states
- Tawfik DS, Profit J, Morgenthaler TI, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018;93(11):1571-1580. doi:10.1016/j .mayocp.2018.05.014
- Karolina Doulougeri, Katerina Georganta & Anthony Montgomery | Albert Lee (Reviewing Editor) (2016) "Diagnosing" burnout among healthcare professionals: Can we find consensus?, Cogent Medicine, 3:1, DOI: 10.1080/2331205X.2016.1237605. Accessed Mar 2020: https://www.tandfonline.com/doi/full/10.1080/2331205X.2016.1237605
- Panagioti, M., Panagopoulou, E., Bower, P., Lewith, G., Kontopantelis, E., Chew-Graham, C., . . . Esmail, A. (2017). Controlled Interventions to Reduce Burnout in Physicians A Systematic Review and Meta-analysis. JAMA Internal Medicine, 177(2), 195-205. doi:10.1001/jamainternmed.2016.7674
- Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, Drop Out, Suicide: Physician Loss in Emergency Medicine, Part I [published correction appears in West J Emerg Med. 2019 Aug 21;20(5):840-841]. West J Emerg Med. 2019;20(3):485-494. doi:10.5811/westjem.2019.4.40970. Accessed Mar 2020: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6526882/
- Kane, Leslie, MA. National Physician Burnout & Suicide Report 2020. Accessed March 2020: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460#5
- 2019 Lifestyle Burnout Depression slides. Medscape. Accessed March 2020: https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#2
- Tuition and Student Fees Reports. Association of American Medical Colleges. Accessed Mar 2020: https://www.aamc.org/data-reports/reporting-tools/report/tuition-and-student-fees-reports
- Panagioti M, Geraghty K, Johnson J, et al. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis [published correction appears in JAMA Intern Med. 2019 Apr 1;179(4):596]. JAMA Intern Med. 2018;178(10):1317–1330. doi:10.1001/jamainternmed.2018.3713: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233757/
- Pauline Anderson. Physicians Experience Highest Suicide Rate of Any Profession. Medscape Medical News. Accessed Mar 2020: https://www.medscape.com/viewarticle/896257