Telehealth and the Hidden Virtues of Virtual Diabetes Care
While telehealth in various forms has been a part of medical care for well over a decade, it has, until recently, received only limited use. Prior to the pandemic, across the U.S. health system, telehealth visits were minimal, representing less than 1% of encounters across all specialties when looking at Medicare telehealth visits.1 However, during the pandemic — as legislative policies expanded coverage for telehealth services, along with improved reimbursement to ease adoption by clinicians — there was a significant increase in physicians who offered remote care services, often in conjunction with face-to-face care to their patients.
By 2020, telehealth visits within the Medicare program represented 8% of primary care visits, and 3% of specialists visits, with the largest increase in visits seen in mental health / behavioral health.1 With Medicare waiving its strict telehealth reimbursement rules, the amount of telehealth services delivered from April to December, 2020 increased tenfold from the previous year, from 5 million to 53 million, according to the U.S. Government Accountability Office.2 At the peak of the pandemic, surveys showed that 32%, or nearly a third, of all outpatient visits were telehealth.3
In the American Medical Association's 2021 telehealth report, over 60% of the clinicians surveyed felt most of their telehealth visits replaced in-person care (63% believed these visits supplemented in person care), with 80% of those providers asserting their patients have better access to care with the use of telehealth.4 85% of the physicians surveyed reported they currently use virtual care, mostly with live video visits, in addition to in person care, and over half want to increase the amount of telehealth they use in their practice.4 Today, telehealth visits are down to an average of 13-17%.3 However, 40% of consumers surveyed by McKinsey, stated they want to continue to use telehealth, significantly higher than the 11% of consumers wanting to use telehealth prior to the pandemic.3
One of the overlooked benefits of the dramatic increase in virtual care during the pandemic is that it gave clinicians the opportunity to use telehealth tools for providing medical care outside of the traditional face-to-face model, and most importantly to evaluate outcomes. The sheer number of telehealth visits also provided real world data for those seeking to study and analyze its impacts on care delivery.
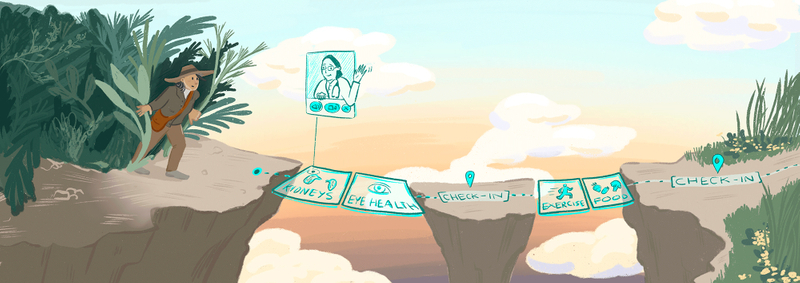
Hybrid Care Delivery
Virtual care has some surprising benefits that build upon what in-person care does well. Telehealth's ability to increase access to medical care by overcoming geographic, time, and mobility barriers makes it a great method to transform how primary care is provided. Combining the traditional face-to-face care in the outpatient clinic with care via a smartphone, tablet, or computer, can ease communication with the patient's health team. More frequent conversations about what patients are eating, how they are moving, and what their life looks like outside of the office visit, can help the health team prevent and treat medical conditions sooner. In this way, telehealth has the potential to make it easier for people to work with their health team and make those healthy lifestyle choices.
Treating Diabetes Virtually
Chronic conditions like diabetes, stroke, and heart disease represent the leading cause for death and disability in the United States, according to the Centers for Disease Control and Prevention.5 Six out of 10 Americans have at least one chronic disease that is often preventable with healthy lifestyle habits.5 Diabetes, in particular, affects 463 million people worldwide.6 In the U.S alone, 37.3 million adults or 11% of the population are diagnosed with diabetes.7 Unfortunately, that includes 8.5 million people who are unaware they have diabetes.7Once diagnosed with diabetes, a person has an increased risk of having other chronic health conditions like obesity, hypertension, heart and liver disease, as well as some forms of cancer. Being able to adequately treat and ideally prevent this condition could potentially prevent many of the chronic health conditions mentioned and promote health and wellness in many communities.
The foundation of care for people with diabetes is two-fold: provide advice and directions on medications (oral agents and insulin injections) for glucose control as well as health education that empowers a patient in the self management of the condition to prevent acute complications and reduce long term complications.8 This type of support has demonstrated an improvement in blood sugar, blood pressure, and weight control for patients with diabetes. Importantly, this usually requires a person with diabetes to have frequent touch points within a comprehensive health system beyond just the physician, including nurses, diabetes educators, nutritionists, or pharmacists.
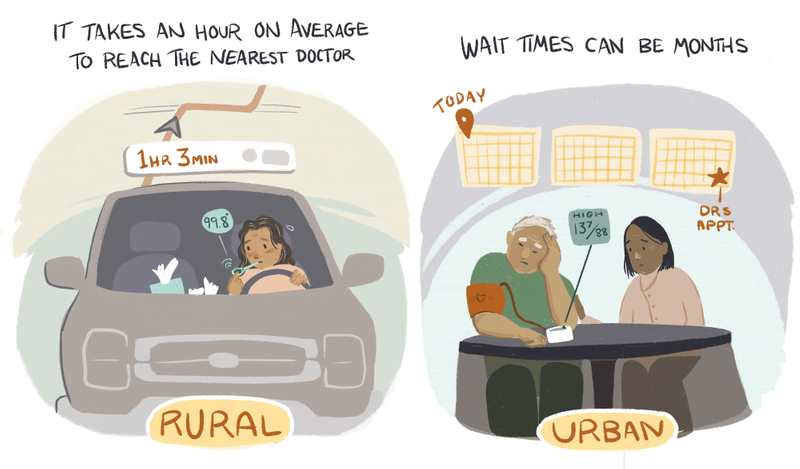
A key resource in providing care to these individuals is time. In rural areas, the commute time to the nearest doctor is an hour on average. In underserved urban areas, the time to an appointment can be months because of the low physician to patient ratios.9
Virtual care delivery alleviates the limitations of face-to-face encounters by creating more touch points and supplementing in person care. Several recent studies show that a virtual managed care system for diabetes can lead to measurable clinical improvements that are similar to those seen with usual face-to-face medical care — including decrease in Hgb A1c, significant and sustained weight loss, and decrease in blood pressure.9,10,11
Clinically, results from a 2021 systematic review and meta analysis of 29 randomized control trials demonstrated when compared to usual care Hgb A1c can be greatly influenced through the use of technology interventions of various types, including telephone, videoconferencing, interactive websites and mobile health apps.11 Additionally, a significant decrease in weight / BMI and blood pressure has also been associated with telemedicine care for diabetes management. A telemedicine program started in the health system of UPMC in Pittsburgh showed an average decrease of A1c from 10.2% to 8.8% in three months.9
Why has hybrid virtual and face-to-face care demonstrated improvement for patients with diabetes?

1. Additional, regular touchpoints can be critical to longitudinal care for chronic diseases like diabetes. Being able to meet virtually means more frequent visits with the physician, diabetes educators, nutritionists, and exercise specialists on the healthcare team, which gives the patient more opportunities to have success within the program and feel empowered. Virtual meetings allow for more frequent touchpoints to closely monitor glucose levels and patient concerns.

2. Virtual care helps patients become active participants in their own care management. A qualitative systematic review of 13 studies showed an improvement in patients becoming active participants in their own care and increasing their self-management skills as elements of virtual care fostered a sense of community, a critical part in being a patient with diabetes.12 Recognizing this, the American Diabetes Association recommends digital coaching and digital self management interventions as effective methods to deliver "diabetes self management education and support".13

3. Virtual care delivery can help shift the focus to preventative care rather than reactive. Virtual care is already playing a significant role in the prevention of diabetes in those most at risk. For example, the diabetes prevention program designed by the CDC is a nationally recognized program focused on lifestyle habits that has been effective in decreasing the risk of Type 2 DM for patients by nearly 58%.14 This program offers a curriculum that focuses on the modifiable lifestyle factors that tend to increase the risk for diabetes — including food choices, physical activity, coping with stress, and resiliency with healthy habits. This is primarily a program conducted in person; however, there are states that offer it online. For instance, North Carolina State University and Blue Cross and Blue Shield of North Carolina have teamed up to host their own virtual program.15 "Eat Smart, Move More, Prevent Diabetes" is recognized as a CDC certified online diabetes prevention program which provides real time instruction with live instructors and evidence based lifestyle strategies to participants.16 This has allowed people to participate from all areas of the state who normally would be limited by time and location.
Extending Longitudinal Virtual Care to Other Chronic Illnesses
Overall, 68% of the medical services provided via telehealth are related to chronic disease management.4 So, it's reasonable to consider that virtual care could have similar positive outcomes for other chronic conditions besides diabetes. Patients with chronic conditions require an integrated system of care that includes the components of "evidence-based, planned care; reorganization of practice systems and provider roles; improved patient self-management support; increased access to expertise; and greater availability of clinical information".17 Virtual and face-to-face care combined in a hybrid model are well-suited to meet these requirements.
Barriers to Virtual Care
There remain a number of barriers to the widespread use of virtual care methods and tools. Despite the evidence suggesting clinical efficacy similar to usual care, digital health as a main foundation for the delivery of diabetes care has not been readily adopted for a number of reasons including: poor reimbursement, unsustainable business models, and patient / provider concerns about private health data security.18
Though insurance reimbursement has expanded since the pandemic, it is inconsistent, and federal agencies, CMS in particular, plan to return to the previous strict regulations that limited its use to a select group of beneficiaries.19 Insurance reimbursement will be a key factor to seeing continuing progress and the positive outcomes for virtual and hybrid care models.
The technology itself is not always accessible or usable by providers and patients. "Poor competence with technology, poor literacy, and language barriers" are common barriers to virtual care.20 In particular, technical issues with mobile apps or virtual video calls will need to be addressed. On the provider side, smaller practices may lack the robust technology to have secure telecommunication during visits and in between.
As with many healthcare technologies and services, access and availability can be an issue. There are fears, perhaps well-founded, that virtual care could further worsen disparities of the more vulnerable populations including the elderly, ethnic minority groups and others in underserved communities.21
Lastly, certain facets of the virtual mode of care will continue to be less desirable to providers. For instance, there are continued concerns about the inability to do physical exams virtually which are important for the management of people with diabetes. Although this particular issue can be mitigated with a hybrid model combining virtual care with face-to-face visits when needed.
A Future of Broader Access and Positive Outcomes
From the evidence gathered in studies over the period of 2020-2021, there are many examples of the benefits of virtual care, especially for difficult to manage chronic conditions like diabetes. Also, over that time period, there has been an important cultural shift related to healthcare: physicians have grown more comfortable with the technology and patients have enjoyed the convenience. While virtual care does have pitfalls, many of these can be mitigated as a part of a hybrid model of medical care, which includes some face-to-face encounters as needed.
If we are moving away from a reactive healthcare approach which often relies on face-to-face evaluations and assessments based on urgency, we need a model of care that allows people to frequently and easily share, talk, and plan with their healthcare team. This hybrid model could represent a paradigm shift that practically allows a preventative approach to healthcare delivery.
Authors
References
- Assistant Secretary for Planning and Evaluation. Medicare Beneficiaries' Use of Telehealth in 2020: Trends by Beneficiary Characteristics and Location. Published December 3, 2021. Accessed December 8, 2022: https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
- U.S Government Accountability Office. Telehealth in the Pandemic- How has it Changed Health care delivery in Medicaid and Medicare? Published September 29, 2022. Accessed December 8, 2022: https://www.gao.gov/blog/telehealth-pandemic-how-has-it-changed-health-care-delivery-medicaid-and-medicare
- Bestsennyy O, Gilber G, Harris A, Rost J. McKinsey & Company. Published July 9,2021. Accessed October 14, 2022: https://www.mckinsey.com/industries/healthcare/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
- American Medical Association. 2021 Telehealth Survey Report. Published March 23, 2022. Accessed October 16,2022: https://www.ama-assn.org/system/files/telehealth-survey-report.pdf
- National Center for Chronic Disease Prevention and Health Promotion. About Chronic Diseases. Updated September 6, 2022. Accessed December 16, 2022: https://www.cdc.gov/chronicdisease/about/index.htm
- Saeedi P, Petersohn I, Salpea P. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019 Nov:157:107843.doi: 10.1016/j.diabres.2019.107843
- Centers for Disease Control and Prevention. By the Numbers: Diabetes in America. Updated October 25, 2022. Accessed December 8, 2022: https://www.cdc.gov/diabetes/health-equity/diabetes-by-the-numbers.html#:~:text=37.3%20million%20people%20have%20diabetes,not%20know%20they%20have%20it
- ElSayed NA, Aleppo G, Vanita, R, et al. Introduction and Methodology: Standards of Care in Diabetes-2023 . Diabetes Care 2023;46(Supplement_1); S1-S4: https://doi.org/10.2337/dc23-Sint
- Saiyed S, Joshi R, Khattab S, Dhillon S. The rapid implementation of an innovative virtual diabetes boot camp program: case study. JMIR Diabetes2022;7(1):e32369. doi: 10.2196/32369: https://doi.org/10.2196/32369
- Al-Badri M, Kilroy CL, Hamdy O, et al. In-person and virtual multidisciplinary intensive lifestyle interventions are equally effective in patients with type 2 diabetes and obesity. Ther Adv Endocrinol Metab 2022: https://doi.org/10.1177/20420188221093220
- Robson N, Hosseinzadeh H. Impact of Telehealth Care among adults living with type 2 diabetes in primary care:a systematic review and meta analysis of randomized controlled trials. Int J Environ Res Public Health 2021 Nov;18(22):12171. doi:10.3390/ijerph182212171: https://doi.org/10.3390%2Fijerph182212171
- Jain SR, Sui Y, Cheng HN. Patients and healthcare professionals' perspectives towards technology-assisted diabetes self-management education. A qualitative systematic review. PLoS One. 2020 Aug 17:15(8):e0237647. doi: 10.1371/journal.pone.0237647
- ElSayed NA, Aleppo G, Aroda V. Facilitating Positive Health Behaviors and Well-Being to Improve Health Outcomes: Standards of Care in Diabetes-2023. Diabetes Care.2023;46(Suppl. 1):S68-S96.doi: https://doi.org/10.2337/dc23-S005
- Centers for Disease Control and Prevention. National Diabetes Prevention Program. Updated December 27, 2022. Accessed October 14, 2022
- Minemyer, P. Blue Cross NC, NC State team on diabetes prevention program. Published September 3, 2021. Accessed October 14, 2022: https://www.fiercehealthcare.com/payer/blue-cross-nc-nc-state-team-diabetes-prevention-program
- Eat More, Move More, Prevent Diabetes. How it works. Accessed October 14, 2022: https://esmmpreventdiabetes.com/how-it-works/
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milibank Q. 1996;74(4):511-44
- Farhad, F. Diabetes Care in the Digital Era: a Synoptic overview. Curr Diab Rep. 2018:18(7) doi:10.1007/s11892-018-1013-5: https://link.springer.com/article/10.1007/s11892-018-1013-5
- Telehealth.HHS.gov. Telehealth policy changes after the covid-19 public health emergency. Updated January 23,2023. Accessed Dec 13 2022: https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/policy-changes-after-the-covid-19-public-health-emergency/#what-is-being-phased-out
- Macleod J, Scher L, Scalzo P. Technology Disparities and Therapeutic Inertia: A Call to Action for the Diabetes Care and Education Specialist. ADCES in Practice. 2021;9(5):34-41. doi:10.1177/2633559X211032227: https://doi.org/10.1177/2633559X211032227


